A review of the week’s plant-based nutrition news 1st May 2022
This week I cover egg consumption and risk of death, plant-based diets for rheumatoid arthritis, low-carb diet and hormone health, meat consumption and inflammatory bowel disease and a blog about my new book.
EGGS, CHOLESTEROL AND RISK OF DEATH: This is the latest study to examine the association between dietary cholesterol, serum cholesterol, egg consumption and the risk of death.
The study included 27,078 Finnish men (who were smokers) followed for 31 years. During this time there were 22,035 deaths of which 9110 were from cardiovascular disease (CVD).
The results showed that each additional 300mg of cholesterol intake per day was associated with a 10% and 13%, higher risk of overall and CVD-related mortality respectively. Each additional 50g egg consumed per day was associated with a 6% and 9% higher risk of overall and CVD-related mortality respectively. Higher serum cholesterol was also associated with a higher risk of CVD mortality and the negative effect of egg consumption was found to be mainly mediated by the impact on serum cholesterol levels.
The study went on to perform a meta-analysis of 41 prospective cohort studies and found a significant positive association for egg consumption and CVD risk in US cohorts, a marginal positive association in European cohorts, and no association in Asian cohorts. The lack significant in Asian cohorts may well be due to their lower lifetime exposure to eggs. They just don’t eat as many eggs as people in the US and Europe!
The authors conclude ‘These findings support restricted consumption of dietary cholesterol as a means to improve long-term cardiovascular health and longevity, and provide compelling evidence relevant to dietary guidelines’.
These results are similar to previous studies, including one from 2019 that included data from 6 prospective US cohorts. You can read a summary of the impact of egg consumption of health outcomes in my book, co-authored with my sister Zahra Kassam.
HEALTHY VEGAN DIET FOR RHEUMATOID ARTHRITIS: There are many compelling reasons why a plant-based diet may benefit people living with rheumatoid arthritis (RA), but to date, only a handful of studies have been conducted. Once again, PCRM have conducted a study that is relevant and adds to the options available for people with RA.
In this study, 44 adults previously diagnosed with RA were randomly assigned to a Diet phase (vegan diet for 4 weeks, elimination of additional foods for 3 weeks, and then reintroduction of the eliminated foods individually over 9 weeks) or a Supplement phase (placebo) for 16 weeks. After a 4-week washout, they switched to the opposite phase. The Diet phase consisted of the elimination of specific foods, followed by their reintroduction, as follows: During weeks 1 through 4, animal products (meat, dairy products, and eggs) were eliminated and added oils were minimised. During weeks 5 through 7, the same exclusions were continued, and the diet was further restricted to eliminate gluten-containing grains (wheat, barley, and rye), soya products, white potatoes, sweet potatoes, chocolate, citrus fruits, nuts and peanuts, onions, corn, tomatoes, apples, bananas, celery, peppers, coffee, alcohol, and table sugar (either separately or as an ingredient). Common staple foods during this period included grains (e.g., rice, oats, quinoa, or millet), vegetables (e.g., broccoli, kale, collards, Brussels sprouts, squash, and carrots), fruit (e.g., pears, apricots, blueberries, or plums), lentils, and beans, all of which could be consumed without restriction. After week 7, the excluded foods were reintroduced, one at a time, every 2 days. Meals were not provided in this study but the participants were supported by the research team. There was no calorie restriction. The placebo Supplement phase involved taking alpha linolenic acid (10 mcg) and vitamin E (10 mcg), doses which would not be expected to result in any clinical benefits.
The results showed that the diet intervention led to significant reduction in disease activity scores as assessed by interviews and physical examination by rheumatologists who were unaware of the patients diet assignment. During the Diet phase, participants also lost a mean of 6.4kg in body weight and had significant reductions in blood cholesterol levels.
The improvements in disease activity are suggested to be due to the anti-inflammatory nature of the plant-based diet, although in this study, there was no significant difference in markers of inflammation between the intervention and placebo group. There is also likely to have been improvement in the gut microbiome, which is implicated in the development of RA.
The main criticism of this study is that you can not tease out the impact of weight loss versus diet change. We know that losing weight will improve symptoms of arthritis and reduce inflammation and of course a plant-based diet is very effective at supporting a healthier body weight. Nonetheless, a plant-based diet is a very reasonable option for people with arthritis bearing in mind these inflammatory conditions also increase the risk of cardiovascular disease and cancer.
LOW-CARBOHYDRATE DIET, CORTISOL AND TESTOSTERONE: It won’t come as a surprise that I am not a fan of the low-carb approach, especially when it emphasises animal sources of protein and fat. I accept there may be short term benefits for weight loss and blood glucose management, but its a potential disaster for long term health with around a third of people getting a rise in LDL-cholesterol level and increasing their risk of cardiovascular disease, cancer and early death. The latest review by the Scientific Advisory Committee on Nutrition in the UK on the use of low-carb diets for management of type 2 diabetes is cautious and only recommends this as a short term approach. This excellent review by PCRM summarises why the low-carb or keto diet is not healthy in the longer term.
The study highlighted assessed the impact of a low-carb diet ob hormone health in men, specifically cortisol and testosterone levels. The analysis included 27 studies, with a total of 309 participants. Low-carb was defined as <35% of energy from carbohydrates and studies included had a least a 20% difference in energy intake from carbs between the intervention and control groups.
The results showed that compared to a high-carb diet, low-carb in the short-term (<3 weeks) moderately increased resting cortisol levels, whereas, long-term (≥3 weeks), low-carb diets had no consistent effect on resting cortisol. This suggests an adaptation phase to the low-carb diet beyond which there may not be any concern. However, a low-carb diet resulted in much higher post-exercise cortisol, after long-duration exercise (≥20 min). This is likely to be due to the fact that glucose supply is limited on a low-carb diet and thus higher cortisol will facilitate glucose production (gluconeogenesis) and preserve glucose availability for the brain. However, higher cortisol levels can also contribute to inflammation and alterations in the immune system.
Regarding testosterone levels, moderate-protein (<35%), low-carbohydrate diets had no consistent effect on resting total testosterone, however high protein (≥35%), low-carbohydrate diets greatly decreased resting (–5.23 nmol/l) and post-exercise total testosterone.
These finding require further investigation as the longer term impact of these endocrine changes (higher post exercise cortisol and lower resting testosterone levels) are not fully understood and there are very few intervention studies on low-carb diets beyond 2 years. However, I believe this should make us cautious with this dietary approach.
This study calls into question the need for meat and high protein diets to be manly. It may be quite the opposite. In contrast, as far as we know, plant-based diets do not have an impact on testosterone levels and lacto-ovo vegetarian diets may lower cortisol levels.
MEAT INTAKE AND ULCERATIVE COLITIS: This is a report from the large European Prospective Investigation into Cancer and Nutrition (EPIC) study and included 413, 593 participants from eight European countries. The study assessed the impact of protein source and intake on inflammatory bowel disease (IBD), both Crohn’s disease (CD) and ulcerative colitis (UC). After a mean follow-up of 16 years, 177 patients with Crohn’s disease (CD) and 418 with ulcerative colitis (UC) were identified. Mean protein intake amongst participants was 87.2g/d. Mean total meat intake in the lowest and highest quartile of consumption was 53.1 and 154.8g/d respectively and for red meat 19.9 and 68.5g/d respectively.
The results did not show an association between total protein intake and risk of CD or UC. However, total and red meat consumption increased the risk UC, with every 10g/d increasing the risk by 5% and those consuming the most increasing their risk by 40%. Meat consumption did not appear to impact the risk of developing CD. The authors conclude ‘This study substantiates the association between meat and red meat consumption and risk of UC. These results support dietary counselling of low meat intake in people at high-risk of IBD’
The key components of the diet that have been implicated in the pathogenesis of IBD are diets high in saturated fat and sugar and low in fibre. The Western-style, meat-heavy diet pattern in particular is associated with a higher risk of IBD. Food additives, including emulsifiers (carboxymethylcellulose and polysorbate-80), maltodextrin (used as thickeners and sweeteners) and carrageenans, used for texture and as thickening agents in the dairy and sauce industry, are also implicated. These adverse dietary factors alter the gut microbiome in an unfavourable way, leading to overgrowth of pathogenic bacteria, reduced bacterial diversity, inflammation and increased intestinal permeability. Interestingly, a recent study 125,445 participants reported that a Western style diet pattern was associated with an increased risk of CD, whereas a Carnivorous, meat heavy diet increased the risk of UC. In a meta-analysis of 9 studies, meat consumption was associated with an increased risk of IBD.
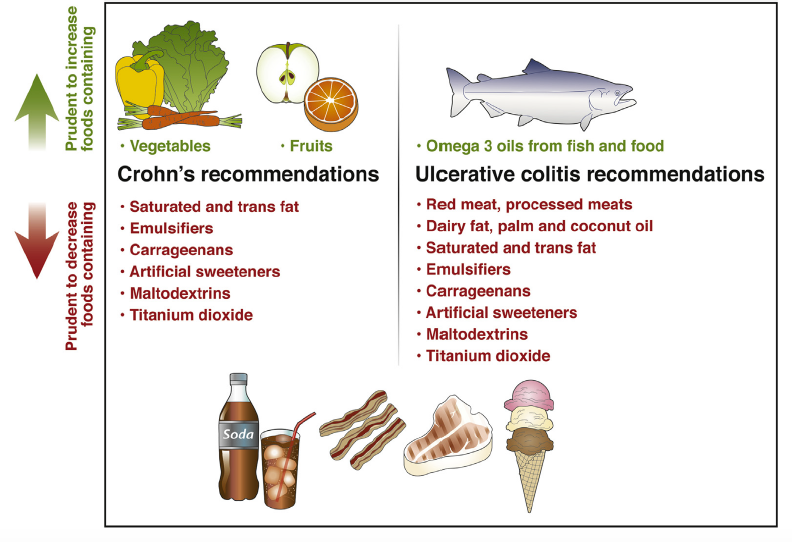
Although, diet does play a significant role in the development of IBD, the study results are not always consistent. Based on the available evidence, the International Organisation for the Study of IBD have produced consensus guidelines. These are summarised in the image below.
Alteration of the gut microbiome is key to the development of IBD and is typically associated with a low abundance of the species responsible for producing short chain fatty acids, specifically butyrate, which has a number of important functions in maintaining the health of the gut and the immune system. This is an excellent and up to date review of the role of gut microbiome in chronic disease, including IBD.
WHY I WROTE A BOOK WITH MY SISTER: Check out this new blog written for The Plantrician Project on why I co-authored a book with my sister. After nearly a decade of discussing the impact of diet choices on health with family, friends and our patients, we wanted to bring together all the commonly asked questions with evidence-based answers in one, easy to access resource. You can check out the book here with access to the first chapter for free.
Please follow my organisation ‘plant-based health professionals UK’ on Instagram @plantbasedhealthprofessionals and facebook. You can support our work by joining as a member or making a donation via the website.
