A review of the week’s plant-based nutrition news 28th August 2022
This week my review is themed around migraine to coincide with the publication of our case series.

PLANT-BASED DIETARY APPROACH: We are excited to see our publication documenting the successful management of migraine headaches using a whole food plant-based approach. I fully accept that this is not high quality evidence, but nonetheless, it provides an option and hope for people suffering from this condition. Migraine headaches are a leading cause of disability globally, ranking second for years lived with disability, with a higher prevalence in women.
The underlying cause is not well understood, but inflammation and oxidative stress are key mechanisms involved. Medications help control the symptoms and prevent attacks but are limited by side effects and do not eliminate the condition. Therefore, a diet and lifestyle approach is attractive. A whole food plant-based diet is known to lower inflammation and oxidative stress whilst reducing the risk of other chronic conditions. In addition, there is increasing recognition of the role of the gut-brain axis in the development of migraine, thus a fibre-rich diet is a sensible approach for optimising gut health.
In 2021, the BMJ reported a dramatic case of migraine remission in a patient who had adopted a whole food plant-based diet with a particular emphasis on dark leafy greens. This attracted media attention.
The three cases described in our series also had dramatic improvements in their migraine headaches with accompanying significant weight loss. They were all able to eliminate or significantly minimise the use of medications and once symptomatic improvement had been achieved, incorporate other healthy habits into their routine.
Please read our open access case series and share with your patients.

RANDOMISED STUDY OF A LOW-FAT VEGAN DIET: The research team at PCRM conducted a randomised cross-over study examining the effects of a low-fat vegan diet intervention on migraine severity and frequency in 42 participants. This 36-week study included two treatments of 16 weeks each. These were 1) dietary instruction and 2) placebo supplement (a mixture of omega-3 oils and vitamin E), with a washout period of four weeks in between. In the diet period, participants were prescribed four weeks of a low-fat vegan diet, then introduced an elimination diet of common triggers whilst continuing the low-fat vegan diet. Significant decreases in reported pain, headache intensity, duration, and percentage of headaches requiring pain relief medication were observed during the diet period compared to the placebo supplement, as well as body weight, total, LDL and HDL cholesterol. There are limitations in this study including teasing out the effect of the elimination diet versus the low-fat vegan diet but certainly suggests that a plant-based dietary approach can be useful for people with migraine.

PLANT-BASED DIETARY PATTERN: I discuss the plant-based diet index frequently, as it is a way of demonstrating the impact of eating healthy plant foods in population studies without the need for large numbers of vegetarian or vegan participants.
This cross-sectional study from Iran used the plant-based dietary index to examine the impact of a healthy plant-based diet on headache severity and duration in 266 women with migraine. A healthy plant-based diet was associated with a significant reduction in headache severity (60% reduction), associated disability (50%) and duration (79%). In contrast, an unhealthy plant-based diet demonstrated an increase in these parameters. As expected, a healthy plant-based diet was associated with higher intakes of fibre, unsaturated fatty acids, vitamin A, C, B6, folic acid, magnesium, potassium, whole grains, vegetables, fruit, legumes, nuts, vegetable oils, and tea/coffee, and a lower intake of energy, protein, carbohydrate, fat, saturated fatty acids, cholesterol, vitamin B12, sodium, sugar-sweetened beverages, refined grains, potatoes, sweets/desserts, dairy, fruits juice, animal fats, and animal-based foods in general. An unhealthy plant-based diet was characterised by higher glycaemic load and index and lower intakes of dietary fibre, micronutrients, and antioxidants.
Once again, this is not a robust study design and hence has a number of limitation. However, the results are consistent with the available data. The authors conclude ‘our findings showed that higher adherence to the plant-based diet, particularly healthy plants, may be associated with lower headache severity, disability and duration. In addition, unhealthy plants may be related with more risk of migraine headaches’.

PLANT FOODS THAT TRIGGER MIGRAINE: Common food and drinks known to trigger migraine include alcohol, coffee and tyramine-rich foods such as processed meat, cheese, and smoked fish. This study examined whether certain plant foods are implicated. Researcher interviewed 3,935 patients with migraine and 1,163 with tension-type headache. Plant-based foods were characterised as triggers of migraine if after single consumption, headache occurred a few hours after ingestion.
The results revealed that certain plant foods trigger headache in 40.3% of people with migraine, but not tension-type headache. Headache was trigger on average 90 minutes after ingestion. The most frequently reported foods were watermelon (29.5%), passion fruit (3.73%), orange (2.01%), pineapple (1.52%), grape (0.51%), banana (0.46%), cucumber (0.43%), acerola (0.25%) and papaya (0.25%). Sour-flavoured fruits were responsible for 8.3% of headache attacks in migraine patients. This has also been observed in previous studies and could be mediated by chemical constituents common to these foods, such as octopamine, a biogenic amine. Regarding watermelon, this fruit is predominantly composed of water (91%). The remainder contains macronutrients (carbohydrates, 6.4%; proteins, 0.5%; fats, 0.2%; and fibres, 0.3%); vitamins (A and B complex), minerals (mostly calcium, phosphorus, magnesium and potassium), bioactive compounds (carotenoids and polyphenols) and citrulline. Citrulline is a non-essential amino acids that is converted to arginine, the precursor to nitric oxide, which is a potent vasodilator. Nitric oxide has been implicated in migraine attacks due to vasodilation of the meningeal arteries. Thus the authors hypothesise that watermelon could trigger headache through the nitric oxide pathway.

OMEGA-3 AND -6 FATTY ACIDS: There are not much data to support the use of supplements for treatment of migraine. The most commonly cited to be of use are magnesium, co-enzyme Q10 and omega-3 fatty acids. Omega-3 and -6 fatty acids are precursors for several families of bioactive lipid mediators that regulate pain. These lipid mediators are collectively known as oxylipins. It is thought that higher intake of omega-3 fatty acids, specifically the long-chain eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA), is associated with reduction in migraine pain whereas higher intake of omega-6 fatty acids has the opposite effect.
This study investigated whether altering the intakes of omega-3 and-6 fatty acids could benefit people with migraine. 182 patients at the University of North Carolina (88% female; average age 38 years), with migraine headaches on 5–20 days per month, were randomly assigned to one of three diets for 16 weeks. The control diet included levels of omega-3 and omega-6 fatty acids typical in the US diet. Both interventional diets raised omega-3 fatty acid intake. One kept omega-6 fatty acid intake the same as the control diet, and the other concurrently lowered omega-6 fatty acid intake. The omega-3 fats were derived from eating fatty fish. Omega-6 intake was lowered by replacing linoleic acids with monounsaturated and saturated fatty acids.
Over the 16 weeks, both interventional diets increased 17-hydroxydocosahexaenoic acid levels (a compound known to reduce pain) compared with the control diet and headache frequency was significantly decreased in both intervention groups. However, there was no benefit for quality of life. The high omega-3 diet was associated with a reduction of 1.3 headache hours per day and two headache days per month. The high omega-3 plus low omega-6 diet group saw a reduction of 1.7 headache hours per day and four headache days per month, suggesting additional benefit from lowering dietary omega-6 fatty acid. Participants in the intervention groups also reported shorter and less severe headaches compared with those in the control group.
The authors conclude, ‘While the diets did not significantly improve quality of life, they produced large, robust reductions in frequency and severity of headaches relative to the control diet’.
I am certainly not advocating for the consumption of fish and the degree of benefit in this study is small, suggesting that it may well be better to concentrate on overall diet quality rather than individual nutrients. However, the study is well designed and conducted and supports the potential benefits of consuming higher amounts of omega-3 fatty acids whilst lower omega-6 fatty acids (found mainly in seed oils and processed foods). It therefore may be worth emphasising this within a plant-based diet by regularly consuming short-chain omega-3 fatty acids from flaxseeds, chia seeds and walnuts. When it comes to omega-3 supplementation, the data are mixed, but there main be some benefit for reducing the duration of headache based on a recent meta-analysis, although omega-3 supplementation did not alter frequency or severity of migraine attacks.
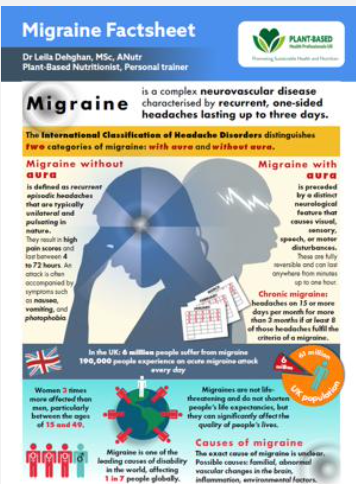
MIGRAINE FACTSHEET: For anyone looking to share this information with patients, clients, friends and family, we have an excellent factsheet covering aspects of diet and lifestyle. We also have an article summarising the evidence.
Please follow my organisation ‘plant-based health professionals UK’ on Instagram @plantbasedhealthprofessionals and facebook. You can support our work by joining as a member or making a donation via the website.
