A review of the week’s plant-based nutrition news 4th December 2022
This week I cover the topic of diet and multiple sclerosis to coincide with the latest publication from our team. We have reported the case histories of two of our members who have successfully used a whole food plant-based diet to manage symptoms and improve quality of life.
Multiple Sclerosis (MS) is an inflammatory and autoimmune condition affecting the brain and the spinal cord. Conventional pharmaceutical treatments slow the progression but rarely reverse or cure it. Observational studies have suggested an increased risk of MS associated with the consumption of a Western diet pattern, high in saturated fat and low in polyunsaturated fats, and with low vitamin D levels. There are two main dietary protocols that are popular with patients living with MS, the Swank diet and the Wahls diet. Here is an excellent summary of these two diet patterns that differ somewhat, and I look forward to the results of the randomised studies. Dr Roy Swank was a proponent of a diet low in saturated fat that limits meat consumption and emphasises fruits and vegetables. His observational study is the longest ever reported on diet and MS following his patients for up to 50 years. The results suggested that patients adhering to a diet low in saturated fat (<20% of calories) had less neurological deterioration. The Wahls study is a modified Paleo diet that emphasises meat, fruits and vegetables but avoids whole grain and legumes due to the lectin content, thought to be associated with increased intestinal permeability and immune activation. Both diets, although quite different, are likely to be healthier than the typical Western diet most patients are eating as both diets avoid processed foods and emphasise ‘real’ whole food and lots of fruits and vegetables. However, avoiding whole grains and legumes eliminates two of the healthiest food groups and I would worry about the longer term risks of cardiovascular disease and cancer, conditions with a higher incidence in people living with MS.
WHOLE FOOD PLANT-BASED DIET FOR MS: We are honoured and proud to have had the opportunity to publish the stories of two of our members who have been managing MS using a whole food plant-based diet. They have both experienced a significant improvement in symptoms and quality of life, allowing for the elimination of medication. We fully appreciate that a plant-based diet is not a ‘cure all’. Nonetheless, people living with MS are often seeking more holistic approaches, and healthcare professionals should be able to support patients to make evidence-based dietary changes.
DIET AND MULTIPLE SCLEROSIS: This study adds to data suggesting that diet choices can make a difference in symptoms for people with MS. This cross-sectional study included 2410 people with MS from the UK MS registry and compared their diet to 24, 852 controls from the East of England. Dietary intakes were correlated with standardised measures of fatigue and health-related quality of life. In particular, these patient-related outcomes were correlated with foods considered to be inflammatory (saturated fat, sodium, sugar, red meat and high-fat dairy products) and anti-inflammatory (carotene, magnesium, oily fish and fruit and vegetables).
The results showed that a better quality diet, lower in saturated fat and higher in fibre was associated with lower levels of disability. In addition, consumption of anti-inflammatory foods was associated with less fatigue and better quality of life. People with MS were more likely than controls to be taking vitamin D and omega-3 supplements and complementary therapies. Higher oily fish intake was also associated with improved symptoms. High red meat consumption was associated with worse fatigue, more pain and worse anxiety and depression. Those consuming the most carotenoids had better overall health and higher consumption of fruits and vegetables was associated with less anxiety and depression and better health. The authors conclude ‘we suggest that a diet rich in anti-inflammatory promoting nutrients and food will contribute to the alleviation of fatigue and in turn improve quality of life for people living with MS’.
Diets rich in anti-inflammatory foods by definition are predominantly plant-based, as anti-inflammatory and antioxidant compounds are only found in plant foods. Anti-inflammatory diets have been associated with a lower risk of a number of chronic diseases, including certain cancers, CVD, type 2 diabetes, mental health illness and cognitive decline. The role of fish consumption for me still remains unclear, as none of the studies confirm fish consumption is necessary but only that it is better than inflammatory foods such as meat, poultry and dairy. Long chain omega-3 fatty acids found in fish can easily be sourced from algae.

DIET QUALITY, MEAT AND MULTIPLE SCLEROSIS: This paper adds extremely useful evidence to the literature. It reports the findings of a prospective analysis of diet and disability, clinically significant fatigue, and depression risk in an international cohort of people with MS followed over a 2.5-year period. The analysis includes 1,346 participants, the majority of whom had relapsing-remitting MS (68%). Interestingly, around 40% of participants did not consume meat or dairy.
The results showed that a higher quality diet with greater consumption of fruits, vegetables and fibre was associated with less disability, fatigue and depression. In addition, the consumption of meat was associated with a significantly increased risk of disability, with dairy also showing some association but not as strong.
There are plausible mechanisms for this finding, the main one being that a fibre-rich diet, low in meat improves the health of the gut microbiome and therefore would have benefits for restoring the immune system. The authors conclude ‘This suggests some promise for healthy and particularly high-fibre plant-based diets in altering the immune profile and thereby moderating clinical progression in MS’. Of course this type of study cannot prove cause and effect, but the results are compelling nonetheless. Prior results from this same study cohort, Health Outcomes and Lifestyle In a Sample of people with Multiple sclerosis (HOLISM), can be found here.
There are a number of anecdotal cases amongst the plant-based community, including our own group, of a plant-based diet improving if not halting the progression of MS.
MEAT HEAVY DIETS, GUT MICROBIOME AND MS: Growing evidence suggests that the health of the gut microbiome is a key factor in the development and profession of MS, given its importance in maintaining a healthy immune system. Diet is the main determinant of gut health with a fibre and polyphenol-rich diet being essential.
In this study, the interaction between diet, the gut microbiome and the immune system was investigated in 25 people living with MS and 24 people without the disease. Gut microbiome composition and function, blood immune cell populations and cytokine profiles were analysed. These results were correlated with a four-day food diary from participants.
A number of differences were found between those with and without MS with adverse changes in the profile of the gut bacteria and immune cells noted. A meat heavy diet was associated with specific changes in the types of gut bacteria present and had an impact on the proportion of certain immune cells. Meat consumption was associated with lower gut levels of Bacteroides thetaiotaomicron — a bacteria involved with digesting carbohydrates from vegetables and producing short chain fatty acids, essential for maintaining immune health. Blood metabolites also differed with methionine being higher, which was consistent with higher meat consumption in the patients studied. Both lower levels of Bacteroides thetaiotaomicron and higher methionine drives T-cell proliferation and differentiation and activates Th17 cells, which are involved in promoting inflammation. The authors suggest ‘meat or methionine restriction might beneficially decrease the number of circulating inflammatory Th17 cells in MS patients’.
A plant-based diet may be key to prevention and management of the condition, likely due to its beneficial effect on the health of the gut microbiome and thus the immune system.
ANTI-INFLAMMATORY DIET AND SYNBIOTICS: This study brings together the concepts have presented so far. That is, an anti-inflammatory diet rich in antioxidant compounds along with a healthy gut microbiome can positively impact outcomes in people living with MS. It is great to have a randomised study putting this to the test. Of note, a synbiotic is defined as a ‘mixture of probiotics and prebiotics’.
The study included 70 patients with different types of progressive MS. Data from 69 patients was analysed, 34 in the intervention group and 35 in the control group. The four-month intervention was a daily synbiotic capsule plus anti-inflammatory-antioxidant rich diet with the control group receiving a placebo capsule plus general healthy dietary recommendations. A trained dietitian designed a personalised anti-inflammatory-antioxidant rich diet, made of 55% carbohydrates, 30% fat (mainly from olive oil, fish, and vegetables), and 15% proteins (restricted for casein & gluten due to proinflammatory properties. The diet included higher intake of major anti-inflammatory and antioxidant food items (extra virgin olive oil, rosemary, thyme, golden raisin, green tea, clove, red pepper, sumac, garlic, ginger); lower calorie intake (1800–2000 kcal/day); and higher fibre content. It did continue to include animal-derived foods. The main study outcomes were an assessment of faecal calprotectin (a marker of intestinal inflammation), changes in vision capacity, gastrointestinal symptoms and anthropometric measurements. Of note, visual symptoms are common in people living with MS due to optic neuritis, chronic optic neuropathy, retrochiasmal visual field defects, and double vision
The results showed that the intervention reduced intestinal inflammation (lowering of calprotectin levels), and improved gastrointestinal symptoms, and vision capacity in patients with progressive forms of MS. However, there was no significant effect on anthropometric measurements. Despite being a small and short study, this does provide proof of principle that dietary interventions that address inflammation and the health of the gut microbiome is feasible and may be of use in people living with MS.
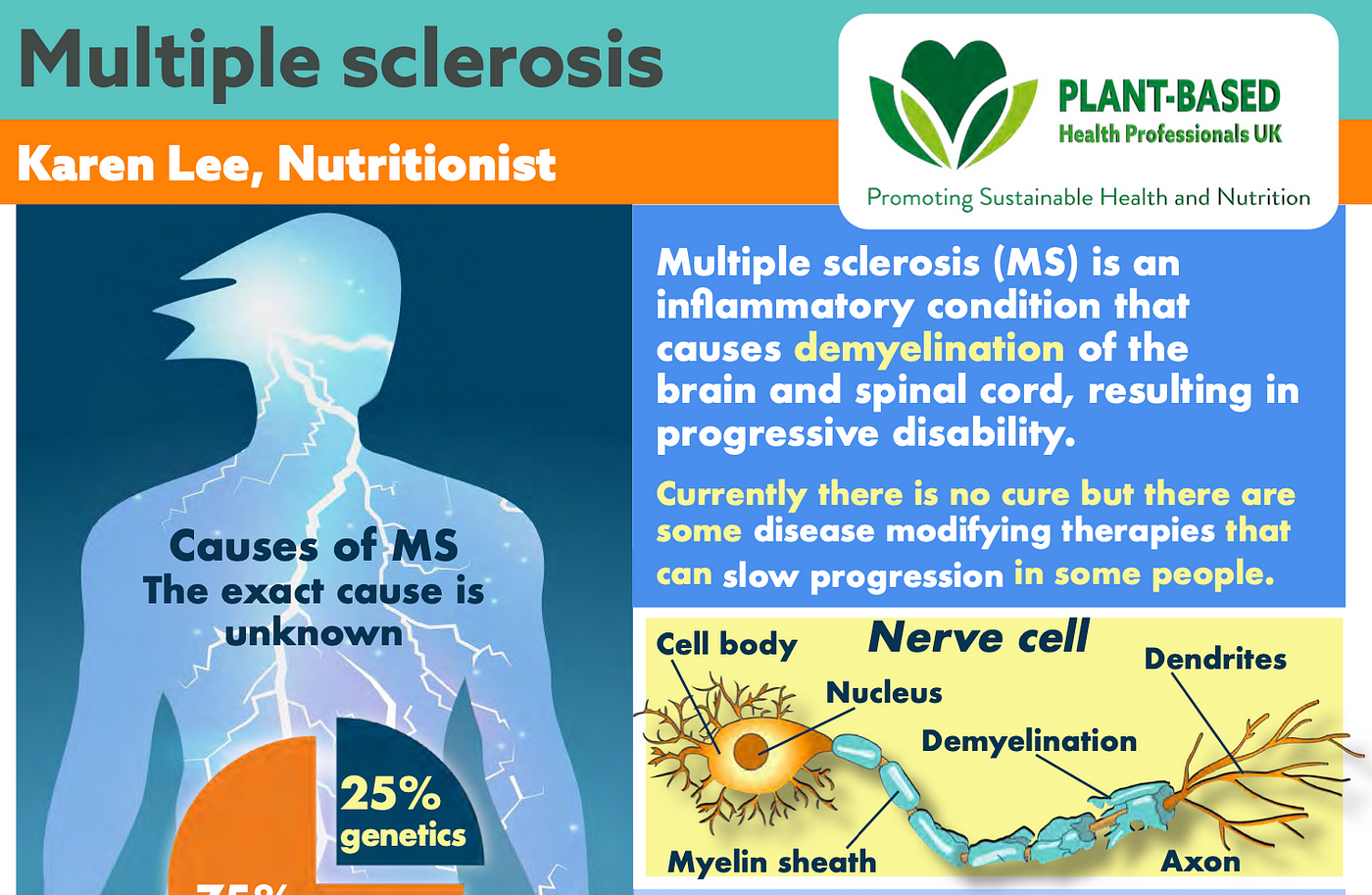
FREE FACTSHEET ON MS: This factsheet was written by Karen Lee, who is featured in our new paper. Another inspiration individual to highlight is Dr Saray Stancic, now working at PCRM, who has documented her remarkable story of healing from MS in the documentary Code Blue and her book What’s Missing From Medicine.
I fully accept that we do not have sufficient evidence to recommend a 100% plant-based diet to all people living with MS. However, what is clear is that focussing on increasing plant-based foods and reducing or eliminating animal-derived and processed foods is the best approach for most people.
Please follow my organisation ‘plant-based health professionals UK’ on Instagram @plantbasedhealthprofessionals and facebook. You can support our work by joining as a member or making a donation via the website.
